We have already seen on the above that the crucial difference between glaucomatous and non-glaucomatous optic atrophy lies in the behavior of glia, especially astrocytes. Under clinical conditions, it is not possible to see or measure astrocyte activation in the optic nerf head. Flammer and coworkers were the first to recognize that activated astrocytes can be detected indirectly in the retina because they backscatter short-wavelength light more intensively than non-activated astrocytes.
We have to distinguish between "epiretinal gliosis" and "gliosis-like alterations." In epiretinal gliosis, glial cells grow over the retina. This has many causes. One of them is hypoxia, mainly as a result of arteriosclerosis and less frequently as a result of vascular dysregulation. Gliosis-like change is an optical phenomenon due to activated astrocytes. This activation can be caused by mechanical stress as well as by changes in blood flow. The cause is less often arteriosclerosis , but more often vascular dysregulation. |
Th Graf, J Flammer, Ch Pnünte, Ph Hendrickson:
Gliosis-Like Retinal Alterations in Glaucoma Patients |
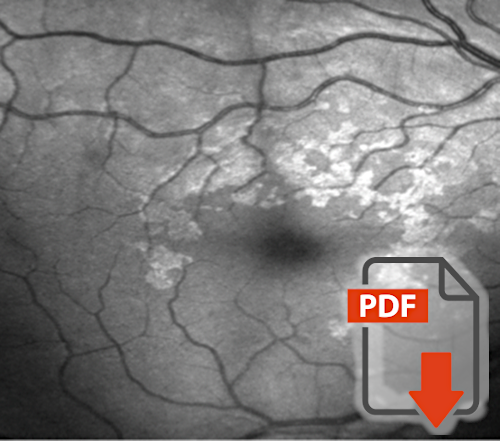
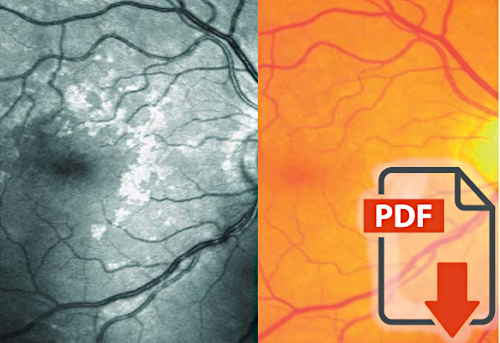
In the 1990s, Graf et al. observed patchy glistening alterations at the fundus, with no known morphologic correlate. Because it had certain similarities to epiretinal gliosis, they called it "gliosis-like retinal alterations". In contrast to true gliosis, the macula was never involved and there were never any distortions of the retina. Accordingly, the patients had no metamorphopsia. The changes were well visible with the help of an argon laser ophthalmoscope, but not on ordinary color photographs. |
MC Grieshaber, S Orgül, A Schötzau, J Flammer:
Relationship Between Retinal Glial Cell Activation in Glaucoma and Vascular Dysregulation |
The "gliosis-like retinal alterations" described above have a distribution pattern like astrocytes. They are absent in the macula and they decrease in density towards the periphery. In addition, no structure could be found in histology that could explain the phenomenon. Therefore, Flammer and coworkers postulated that it must be an increased backscattering by activated astrocytes. In the present work, Grieshaber et al. show that this phenomenon is significantly more frequent in patients with primary vascular dysregulation. |