Glaucoma patients, especially those with normal tension glaucoma often have optic disc hemorrhages. These hemorrhages are localized in the retina at the edge of the optic disc, are flame-shaped (because they spread in the nerve fiber layer), recur and are often followed by an increase in glaucoma damage. However, very many things are still unclear about this, such as which vessels it bleeds from or whether it is a result of vascular rupture, etc.
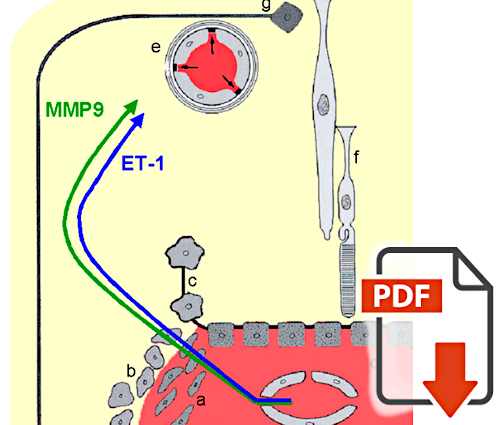
Flammer and coworkers have shown that vasoactive molecules diffuse from the choroid into this area and weaken the blood-brain barrier and the basement membrane of the vessels. This leads to leakage and occasionally opens the barrier to such an extent that even blood cells can leak out (see Flammer et al.: Basic Science in Ophthalmology; or Flammer and Konieczka: The discovery of the Flammer syndrome). |
MC Grieshaber, T Terhorst, J Flammer:
The pathogenesis of optic disc splinter hemorrhages: a new hypothesis |
Fluorescein angiographic studies show mild leakage in and around the optic nerve head of glaucoma patients. This is also the region where optic disc rim hemorrhages frequently occur. Flammer's group was the first to postulate that such optic disc rim hemorrhages in glaucoma were the result of a barrier disorder. In this paper, Grieshaber et al. present evidence that such hemorrhages occur with or without glaucoma, particularly in barrier disorders associated with primary vascular dysregulation. |
MC Grieshaber, J Flammer:
Does the Blood-brain Barrier Play a Role in Glaucoma? |
The optic nerve is part of the central nervous system and therefore has a blood-brain barrier. Interestingly, the optic nerve head is an exception. The so-called Elschnig tissue does not completely separate the optic disc from the fenestrated peripapillary choriocapillaris. In addition, the capillaries in the prelaminar layer have an only partially formed barrier. This allows larger molecules to bypass the blood-brain barrier, which makes this tissue particularly exposed. As shown in this review by Grieshaber et al, this allows endothelin to partially open the endothelial cell barrier and MMP-9 to partially open the basement membrane barrier, leading to hemorrhage. |