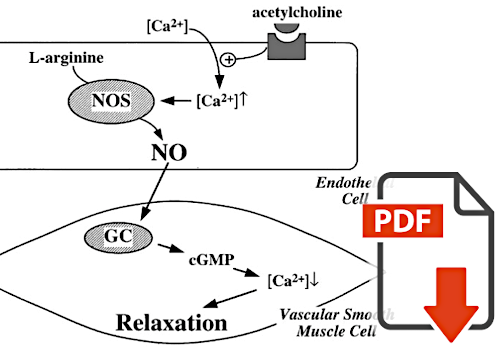
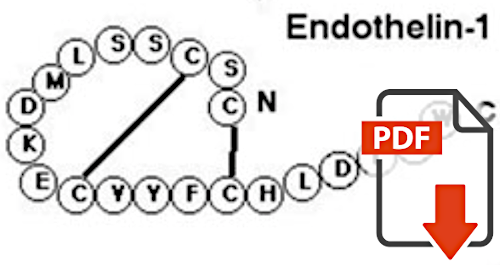
| In the past, it was assumed that blood flow was mainly regulated by the autonomic nervous system. In the 1970s, it was recognized that vascular endothelial cells play a decisive role in regulation. In the early 1980s, Flammer's research group investigated the role of these endothelial cells in the regulation of ocular blood flow and described, among other things, the great importance of NO (nitric oxide) and ET (endothelin). This is particularly interesting because the blood vessels of the retina and optic disc are not autonomously innervated. |
IO Haefliger, J Flammer, TF Lüscher:
Nitric Oxide and Endothelin-1 ore Important Regulators of Human Ophthalmic Artery |
Häfliger et al. have found that the human ophthalmic artery is regulated by local nitric oxide (a vaso-dilator) and endothelin (a vaso-constrictor) generated in the vascular endothelial cells. Thus, they have shown that ocular blood supply is regulated at all levels, including the feeding vessels behind the eye. Thus, the possibility or risk of vascular dysregulation is also present, especially in pathological processes involving the vascular endothelial cells. |

I0 Haefliger, J Flammer, TF Lüscher:
Heterogeneity of Endothelium-Dependent Regulation in Ophthalmic and Ciliary Arteries |
Häfliger et al. have shown that all ocular blood vessels are regulated in the same way by vasoactive substances from the vascular endothelial cells. However, the extent of this regulation is heterogeneous from blood vessel to blood vessel, and the smaller the vessels, the greater the influence of these vasoactive substances on vascular tone. This then also explains why vascular dysregulation manifests itself more strongly in certain vessels than in others. |
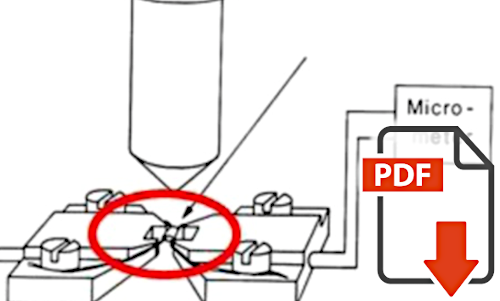
P Meyer, J Flammer, TF Lüscher:
Local Anesthetic Drugs Reduce Endothelium-Dependent Relaxations of Porcine Ciliary Arteries |
Regulation of blood flow by vascular endothelial cells explains not only pathologic processes, such as vascular dysregulation, but also certain drug effects. It has long been suspected that retrobulbar anesthesia may transiently reduce ocular blood flow and thus be detrimental during glaucoma surgery. While this was previously explained by mechanical compression of the vessels in the orbit, Meyer al. have shown that local anesthetics inhibit the formation of nitric oxide and thus cause vasoconstriction. |
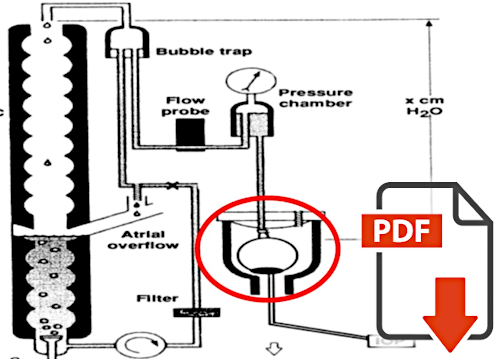
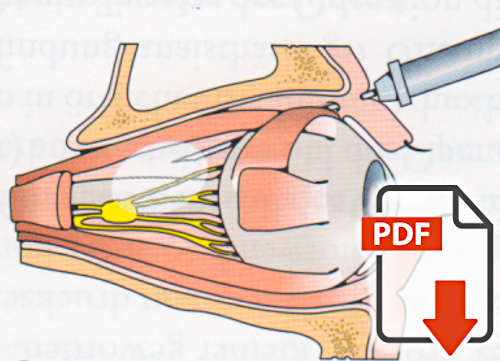
P Meyer, J Flammer, TF Lüscher:
Endothelium-Dependent Regulation of the Ophthalmic Microcirculation in the Perfused Porcine Eye: Role of Nitric Oxide and Endothelins |
The first insights into the regulation of ocular blood flow by vascular endothelial cells were obtained from studies on isolated blood vessels from animals and humans. Meyer et al. isolated and perfused entire eyes from slaughtered pigs. This allowed them to study the regulation of blood flow in an organ as a whole. They have verified that the findings on the role of vascular endothelial cells, obtained on individual blood vessels, can be transferred to the entire organ eye. |
IO Haefliger, J Flammer, JL Bény, TF, Lüscher:
Endothelium-dependent Vasoactive Modulation in the Ophthalmic Circulation |
In the 1990s, it became clear that in addition to the two main players in endothelial regulation, namely endothelin and nitric oxide, many other factors produced by the endothelial cells are also involved, e.g. prostaglandins. The Flammer group has studied this systematically regarding the blood flow in the eye. We show here a review of the regulation of ocular blood flow by vascular endothelial cells by Häfliger et al. |
N Pelllanda, J Flammer, IO Haefliger:
L-Name- and U 46619-induced contraction in isolated porcine ciliary arteries versus vortex veins |
For a long time, it was thought that local blood flow was regulated by arteries and arterioles and that veins played only a passive role. Pellanda et al. showed that vortex veins are regulated as much by endothelial factors as, for example, ciliary arteries. This finding was one of the bases for Flammer's theory on the regulation of retinal venous pressure and the development of retinal vein occlusion, but also for the dysregulation of the veins in the choroid of patients with central serous chorioretinopathy described by Prünte and Flammer. |
M Emre, S Orgül, T Haufschild, SG Shaw, J Flammer:
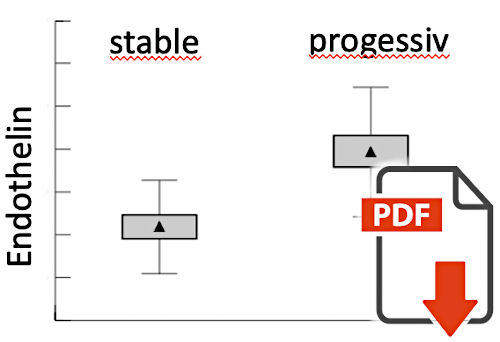
Increased plasma endothelin-1 levels in patients with progressive open angle glaucoma |
Emre et al. showed that plasma levels of endothelin-1 were significantly increased in glaucoma patients who experienced progressive visual field loss despite normal or normalized intraocular pressure. Although the exact role of endothelin in glaucoma was not clear at that time, it clearly showed that a) blood flow plays a role in the pathogenesis of glaucoma damage and b) that the vascular aspects are not simply the same in all glaucoma patients. |
A Gass, J Flammer, L Linder, SC Romerio, P Gasser, WE. Haefeli:
Inverse correlation between endothelin-1- induced peripheral microvascular vasoconstriction and blood pressure in glaucoma patients |
The vascular response to endothelin depends not only on endothelin concentration but also on endothelin sensitivity. This sensitivity varies locally and varies over time. Gass et al have shown that in glaucoma patients, endothelin sensitivity becomes greater with decreasing blood pressure. This inverse relation between endothelin sensitivity and blood pressure is important if we are to understand the role of blood pressure in the development of glaucoma damage. Patients with anterior ischemic optic neuropathy (AION) do not develop glaucomatous but bland optic disc atrophy after the acute event. Flammer and coworkers had shown that patients with giant cell arteritis were an exception to this rule. Later, the same group showed that patients with such giant cell arteritis have a substantial transitory increase in blood endothelin levels, which explains the similarity to glaucoma. |
M Pache, HJ Kaiser, T Haufschild, P Lübeck, J Flammer:
Increased Endothelin-1 Plasma Levels in Giant Cell Arteritis: A Report on Four Patients |
Patients with anterior ischemic optic neuropathy (AION) do not develop glaucomatous but bland optic disc atrophy after the acute event. Flammer and coworkers had shown that patients with giant cell arteritis were an exception to this rule. Later, the same group showed that patients with such giant cell arteritis have a substantial transitory increase in blood endothelin levels, which explains the similarity to glaucoma. |
IO Haefliger, J Flammer:
Nitric oxide and Endothelin in the Pathogenesis of Glaucoma |
Flammer's group had organized the "Glaucoma-Meeting Basel" annually throughout his chairmanship and subsequently published many of the lectures in book form. One example is the book on "Nitric oxide and Entothelin in the Pathogenesis of Glaucoma", edited by Haefliger and Flammer, published in 1998. It summarizes the state of knowledge at that time about the role of these two important molecules in glaucoma. |