| Retinal venous pressure (RVP) is the blood pressure in the veins of the retina, sometimes it is also called central retinal vein occlusion pressure. RVP can be elevated in many different diseases. These include retinal vein occlusion, diabetic retinopathy, macular edema, central serous chorioretinopathy, altitude sickness but also glaucoma and especially normal tension glaucoma. This means that RVP is often significantly higher than intraocular pressure. This plays a very important role in the development and progression of glaucoma damage. Therefore, it is crucial to measure the RVP and treat it if elevated. |
J Flammer:
Retinal venous pressure, pathophysiology and clinical relevance (Video) |
In this video, Josef Flammer illustrates all aspects of retinal venous pressure (RVP), e.g. what the RVP is in healthy people and in which diseases it increases. Based on his team's own research, he explains the mechanisms that lead to this increase. High RVP has many consequences. Among other things, it decreases perfusion pressure and increases transmural pressure. This increases the risk of hypoxia in the optic disc in glaucoma patients or the risk of edema in the retina in patients with diabetes. This is particularly important as a high RVP can be lowered in most cases. |
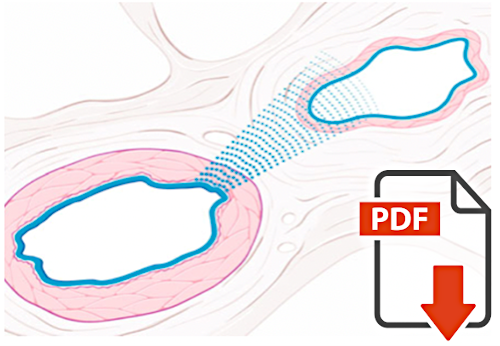
J Flammer, K Konieczka:
Retinal venous pressure: the role of endothelin |
Based on an analysis of scientific studies and clinical observations, Flammer and Konieczka were the first to hypothesize that retinal venous pressure (RVP) is actively regulated, at least in part. This is done primarily by endothelin and other vasoconstrictors. When these molecules are able to bypass the blood-retinal barrier and reach the vascular smooth muscle cells directly, the veins constrict locally, thereby increasing RVP. |
SA Fraenkl, M Mozaffarieh, J Flammer:
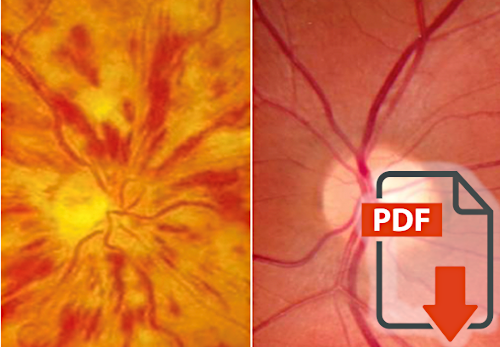
Retinal vein occlusions: The potential impact of a dysregulation of the retinal veins |
Frankl, Mozaffarieh, and Flammer were the first to formulate the hypothesis that retinal vein occlusion can result from active constriction of a retinal vein. The common theory that such occlusion is the result of venous thrombus cannot explain many clinical and scientific findings. And local narrowing of retinal veins used to be explained also by mechanical compression. This conception also cannot explain many phenomena. The new hypothesis is described and substantiated in this PDF. |

L Fang, M Bärtschi, M Mozaffarieh:
The effect of Flammer-syndrome on retinal venous pressure |
Retinal venous pressure (RVP) is increased in various diseases, e.g. normal tension glaucoma. However, an elevation can also be found in healthy people with certain predispositions. This includes Flammer syndrome (FS). FS is also a risk factor for normal tension glaucoma (NTG). Consistent with this, Fang and coauthors found the greatest difference between RVP and IOP in the group of people who had both NTG and FS. |
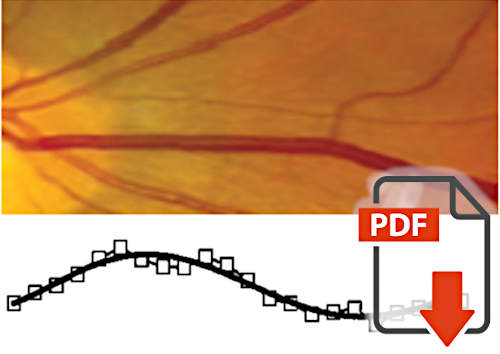
M Ghanem, K Gugleta A Oettli A Kochkorov, A Polunina, J Flammer, S Orgül:
Analysis of Retinal Vein Motion in Glaucoma Patients |
In times when we could not measure venous pressure, enlarged diameters of the veins were observed in various diseases, e.g. glaucoma. As Ghanam et al. describe here in this paper, one can also observe decreased pulse amplitude of the vein as an indication of impaired venous outflow. This demonstrates that such vascular findings can only be interpreted correctly in combination with retinal venous pressure. |
M Mozaffarieh, M Bärtschi, B Henrich, A Schötzau, J. Flammer:
Retinal venous pressure in the non-affected eye of patients with retinal vein occlusions |
That retinal venous pressure (RVP) is elevated in eyes with retinal vein occlusion is not surprising. Mozaffarieh et al. have shown that RVP is also increased in the clinically healthy partner eye. This seems surprising at first glance, but it can be explained by the increased endothelin plasma level in patients with retinal vein occlusion. The increased endothelin in the circulating blood locally constricts the vein in and around the optic nerve head and increases the RVP and in extreme cases even leads to the clinical picture of retinal vein occlusion. |
K Konieczka, St Fraenkl, M Mozaffarieh, J Flammer:
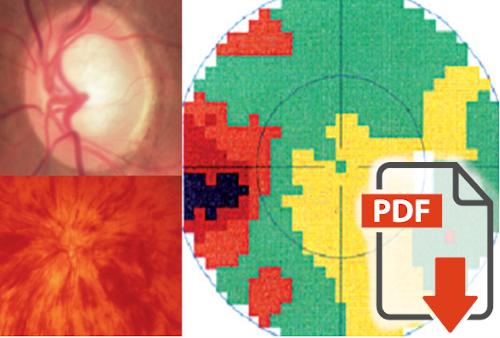
Glaucoma Progression in the Unaffected Fellow Eye of Glaucoma Patients who Developed Unilateral Branch Retinal Vein Occlusion |
Glaucoma patients with unilateral retinal vein occlusion have a more rapid progression of glaucoma damage in the fellow eye (without occlusion) than glaucoma patients without vein occlusions. Konieczka et al. have published a plausible explanation for this: Patients with unilateral venous occlusions have increased endothelin levels and thus increased retinal venous pressure in the fellow eye. Among other things, this reduces perfusion pressure and thus explains the faster progression. |

M Baertschi, P Dayhaw-Barker, J Flammer:
The effect of hypoxia on intra-ocular, mean arterial, retinal venous and ocular perfusion pressures |
Retinal venous pressure (RVP) is elevated in many diseases. For a long time, it was thought that this was always a consequence of mechanical compression of veins. The hypothesis of Flammer that this is mainly a consequence of an active constriction of the veins has been confirmed by the work of Baertschi et al. In fact, they observed that even in completely healthy mountain climbers, RVP increases as a function of altitude. Low oxygen concentration increases HIF1-alpha and thus also endothelin, which then induces local constriction of retinal veins in and around the optic nerve head. |
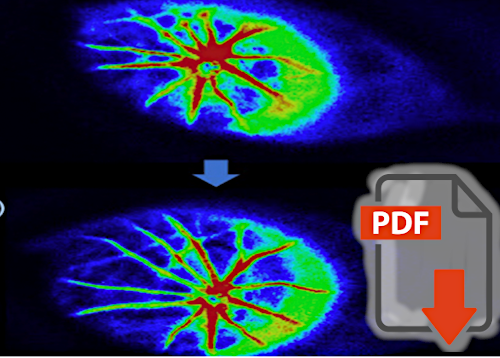
T Kida, J Flammer, H Oku, K Konieczka, S Morishita, T Horie, T Ikeda:
Vasoactivity of retinal veins: A potential involvement of endothelin-1 (ET-1) in the pathogenesis of retinal vein occlusion (RVO) |
Flammer had formulated the hypothesis that endothelin circulating in the blood can lead to a constriction of the retinal veins in and around the optic nerve head and thus to an increase of the retinal venous pressure. In extreme cases, this even leads to the clinical picture of retinal vein occlusion. This has been definitely demonstrated by Kida and coauthors. They have experimentally shown that intravenous infusion of endothelin constricts the veins in the optic disc. In addition, they have shown that spontaneously hypertensive rats have a higher endothelin sensitivity. This is one explanation why arterial hypertension is a risk factor for retinal vein occlusion. |
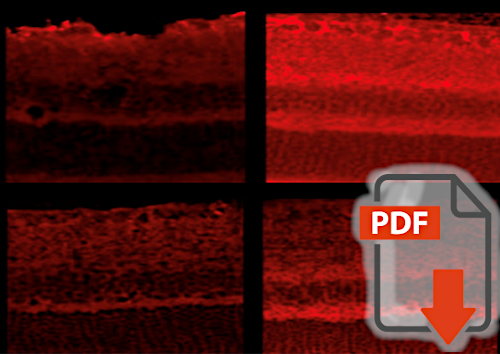
T Kida, J Flammer, H Oku, K Konieczka, S Morishita, T Horie, T Ikeda:
Data on the involvement of endothelin-1 (ET-1) in the dysregulation of retinal veins |
Endothelin locally constricts the retinal veins. This endothelin may diffuse from the choroid into the optic disc or originate from adjacent diseased retinal arteries. In addition to endothelin concentration, endothelin sensitivity also plays a role. Kida et al. have shown that spontaneously hypertensive rats express more ET-A receptors and have a higher level of HIF 1-alpha than healthy rats. This explains on the one hand the risk constellation for retinal vein occlusion and on the other hand the theory of Flammer, according to which endothelin is involved in the regulation of retinal vein pressure as well as in the genesis of retinal vein occlusion. |